Biventricular Pacemaker and ICD (Biventricular ICD)
You have a condition called heart failure. This condition causes symptoms such as getting tired very quickly and being short of breath. To help treat these symptoms, your healthcare provider is recommending a biventricular pacemaker and implantable cardioverter defibrillator (ICD). This is sometimes called a biventricular ICD. It's also called cardiac resynchronization pacing with an ICD (CRT-D). A biventricular pacemaker and ICD is a small, lightweight device powered by batteries. This device helps keep your heart pumping normally. It also protects you from dangerous heart rhythms.
Understanding the heart
The heart is made up of four chambers that pump to move blood through the heart. The top two chambers are the left atrium and right atrium. These are filling chambers of the heart. The bottom chambers are the left ventricle and right ventricle. These are the pumping chambers of the heart. Heartbeats are electrically generated within the right atrium from a structure called the sinus node. This electrical signal is then transmitted from the atria to the ventricles over specialized conduction pathways called the AV node and bundle branches. These bundle branch pathways extend into the left and right ventricles and allow coordinated contraction of the left and right ventricle.
How the device works
People with heart failure often have damaged or weakened heart muscle in the ventricles. The bundle branch pathways that run through the heart muscle can also be damaged, resulting in uncoordinated timing of the left and right ventricles. As a result, the ventricles don’t pump as efficiently as they should, making the heart's squeezing contraction even weaker.
A biventricular pacemaker and ICD help keep the heart pumping in a more normal way. The pacemaker keeps the heart from beating too slowly. It tries to restore the normal squeezing pattern of the heart by coordinating left and right heart contraction. This is called resynchronization pacing. This can lead to more efficient and stronger heart contraction. The ICD part of the device detects dangerously fast heart rhythms and attempts to terminate them with either pacing or delivering a shock. The bursts of pacing or delivery of a shock often stops this dangerous heart rhythm and restores a normal heartbeat.
Before the procedure
Make sure to:
-
Follow any directions you are given for not eating or drinking before surgery.
-
Follow instructions from your healthcare provider about bathing the night before and the morning of your procedure. You may need to use a special cleaning solution.
-
Tell your healthcare provider what medicines you take. This includes over-the-counter medicines such as ibuprofen. It also includes vitamins, herbs, and other supplements. You may need to stop taking some medicines before the procedure, such as blood thinners and aspirin.
-
Tell your healthcare provider if you are sensitive or allergic to anything. This includes medicines, latex, tape, and anesthetic medicines.
-
Ask a family member or friend to take you home from the hospital.
Tests before your procedure
Before your procedure, you may need tests such as:
-
Chest X-ray
-
Blood tests, to test your general health
-
Echocardiogram to assess your heart's function and electrocardiogram to assess your heart rhythm
During the procedure
-
You will get medicine (anesthesia) so you won’t feel pain. Most likely, you will get medicine (sedation) that will make you drowsy or lightly asleep. The healthcare provider will inject local pain medicine to numb the skin on your chest where the cut (incision) will be made.
-
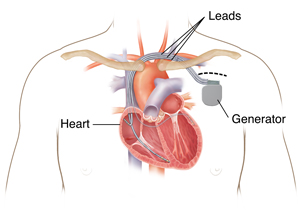
The healthcare provider will make an incision where the device will be implanted. This is most often on the left side of the chest just below the collarbone.
-
The healthcare provider makes a small “pocket” for the generator under the skin.
-
The healthcare provider will put a thin, flexible tube (catheter) into a vein leading to the right atrium. They will guide the device’s wires (leads) through the catheter to the heart. The doctor will use an X-ray monitor to move the leads into the right ventricle. They will usually also put a lead in the right atrium.
-
The healthcare provider will put the lead for the left ventricle into a vein that runs along the outside of this chamber. They will also use the X-ray monitor to put this lead in the correct spot. The device will stimulate the left ventricle from the outside. The other leads will stimulate the heart from inside the chambers.
-
The healthcare provider will attach the generator to the leads. They will send pulses through the leads to test the generator. This testing may cause your heart to race.
-
The healthcare provider will then put the generator into the pocket under your skin.
-
The healthcare provider will program the device based on the heart rate that’s best for you. They will check the device to see that it's working.
-
The healthcare provider will close the skin with stitches, surgical glue, or staples. Any stitches used will likely dissolve on their own over time. If glue is used, it will seal the cut and prevent infection. A bandage will be put on the area.
After the procedure
You will spend several hours in a recovery room. Once you are stable and awake, you will be put in a room that can monitor your heart rhythm. Your healthcare team will also watch your breathing and other vital signs. You’ll be given pain medicine if you need it.
The team may place the arm on the side of the device in a sling. This is just for a short time, to keep the arm and shoulder still.
You will have a chest X-ray to make sure the leads are where they should be. The healthcare provider will also check that your lungs were not injured during the procedure.
You can resume a normal diet as soon as you are able. You will be watched overnight. The team will check the device the next morning. You will likely go home the day after your procedure. You may need to take antibiotics for several days to prevent infection.
Recovering at home
Follow all the instructions your healthcare provider gives you for medicines, bathing, exercise, diet, and wound care. Ask your healthcare provider when you can go back to work or start driving again.
Don’t raise your arm above your shoulder on the side of your incision until your healthcare provider says it’s OK to do so. Usually this is in about 3 to 4 weeks. This gives the leads a chance to secure themselves inside your heart.
Follow-up care
Make sure to keep all your follow-up appointments. This is so your healthcare provider can download information from your device and check its settings. Be sure to tell your healthcare provider how the device is working for you.
Most devices can now be connected to a wireless home monitoring system via the Internet. The monitor can download information from your device and send it to your healthcare provider. This lets your healthcare provider make sure the device is working as it should.
Life with a biventricular pacemaker and ICD
-
Carry an ID card. When you first get your device, you’ll be given an ID card to carry. This card contains important information about the device. Show it to any doctor, dentist, or other healthcare provider you visit. Pacemakers may set off metal detectors. So you may need to show your card to security personnel.
-
Be careful when using a cell phone and other electronic devices. Keep them at least 6 inches away from your pacemaker or ICD. It's safest to hold all cell phones to the ear farther from your pacemaker or ICD or use the speaker mode setting. Don’t carry your phone or electronic device in your chest pocket, over the pacemaker or ICD. Experts advise carrying your cell phone and other electronics in a pocket or bag below your waist. Most cell phones and electronic devices don't interfere with pacemakers or ICDs. But some cell phones and electronic devices such as smartwatches use powerful magnets for wireless charging. These may interfere with the normal function of your pacemaker or ICD. The magnet used for charging or other magnet accessories can also interfere with the normal function of your pacemaker or ICD. These devices should be kept away from your pacemaker or ICD when wirelessly charging or stored. Follow any other instructions given to you by your healthcare provider or from the manufacturer of your pacemaker or ICD.
-
Stay away from very strong magnets. Most modern devices are compatible with MRI machines but may need to be reprogrammed before undergoing an MRI scan. When going through security screening such as at an airport, show your ID card to security so that they can take the proper precautions for your device during screening.
-
Stay away from strong electrical fields. Some electrical generators may create enough electromagnetic interference to affect the normal function of your device. Avoid direct contact or being in close proximity to industrial generators. Most household and yard appliances will not cause any problems. Avoid touching the engine block of a running car engine. If you use any large power tools, such as an industrial arc welder, talk to your healthcare provider.
-
Keep an eye on the battery. The battery inside the device is checked regularly. It will generally last 10 years or possibly longer, depending on how often it paces or has to stop dangerous heart rhythms. Once it starts to run down, you will need to have it changed. This is like the implantation surgery, but it takes less time. This is because typically the battery/generator is the only part that needs to be replaced.
-
Be careful when driving. Your device has a defibrillator built in. It's recommended that you avoid driving for as long as your healthcare provider advises after implant. You may also not be allowed to drive for a period of time after the defibrillator delivers a shock or if you had a prior episode of cardiac arrest. You will not be allowed to work as a commercial driver if you have an ICD.
When to call your healthcare provider
Call 911 if you have chest pain, trouble breathing, or feel like you might pass out.
Call your healthcare provider if you have any of the following:
-
Redness, severe swelling, severe pain, drainage, bleeding, or warmth at the incision site
-
Incision site or opens up or does not heal well
-
A fever of 100.4°F (38°C) or higher (or 1 degree or higher above your normal temperature) , or as directed by your healthcare provider
-
Pain around the generator that gets worse
-
Swelling in the arms or hands on the side of the incision
-
Sudden weight gain
-
Twitching chest or abdominal muscles
-
Frequent or constant hiccups
-
A shock from your device
-
Very fast heartbeat that doesn’t stop
-
Generator feels loose or like it is wiggling in the pocket under the skin