Open Mitral Valve Repair
What is open mitral valve repair?
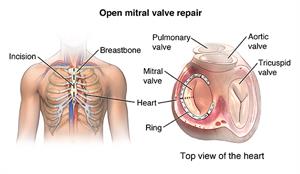
The heart has 4 valves. These valves help blood flow through the heart and out to the body by helping the blood flow forward and not letting it flow backward.
Your mitral valve is a small but essential part of your heart. The valve lies between the 2 chambers of the heart on the left side. These 2 chambers are the left atrium and left ventricle. When the valve is open, it lets blood flow from your lung and left atrium to your left ventricle, the main pumping chamber of the heart. When the left ventricle contracts to pump blood into your body, the mitral valve closes to prevent blood from leaking backward. If your mitral valve is deformed, becomes damaged, or doesn’t work correctly, you may need surgery to repair it.

Open-heart surgery is the traditional procedure used to repair the mitral valve. This involves a deep cut (incision) that goes through your breastbone. There are other less invasive valve repair options available now.
Why might I need an open mitral valve repair?
The most common reason for mitral valve repair surgery is to correct a leaking valve, also known as mitral regurgitation or mitral insufficiency.
This leaking can occur because of a heart defect you were born with, damage from a heart attack, advanced age, or a bacterial infection in your valve.
Sometimes, a mitral valve needs to be repaired because it's too stiff to open correctly (mitral stenosis). You might have been born with this stiffness, but it can also be caused by damage from rheumatic fever.
In general, the outcome is better when a surgeon repairs, rather than replaces, your mitral valve. But if your valve has too much damage, your surgeon may need to replace it. Your healthcare provider will perform tests before your surgery to decide which treatment is best for you.
What are the risks for an open mitral valve repair?
Open mitral valve repair is major surgery that requires general anesthesia. This means the anesthesiologist will give you medicine to make you fall asleep and prevent you from feeling any pain. Any general anesthesia involves risks, including the risk of heart or brain injury. Major surgery also carries the risk of blood clots forming during or after surgery. These clots can break free and travel to your lungs, causing a pulmonary embolism. They can also travel to your brain, causing a stroke or blocking blood flow as the clot becomes lodged in other vessels.
Other risks of this surgery include:
-
Infection, including in the lungs (pneumonia), in the wound, and in the heart
-
Bleeding, which may require blood transfusion in some cases
-
Damage to nearby organs
-
Irregular heartbeats (arrhythmia), which may require a permanent pacemaker
-
Reaction to medicine, including allergic reactions
-
Memory loss or problems with concentration
-
Need for more surgery
-
Problems with mitral valve functioning
-
Heart attack
-
Stroke
-
Death
There may be other risks, depending on your specific health condition. Discuss any concerns with your healthcare provider before the procedure.
How do I get ready for an open mitral valve repair?
Before mitral valve repair surgery, your healthcare team will conduct a complete evaluation to figure out the repairs that you'll likely need. You'll probably have a transesophageal echocardiogram (TEE). This is an imaging test done through your esophagus to better visualize your valve.

In addition:
-
Your surgeon will explain the procedure. Use this time to ask questions.
-
You'll be asked to sign a consent form that gives your permission to do the test. Read the form carefully and ask questions if something isn't clear.
-
In addition to a complete health history, your surgeon may request a complete physical exam to ensure you are in good health before undergoing the procedure. You may have blood tests or other diagnostic tests.
-
Follow any directions you're given for not eating or drinking before surgery.
-
You may be asked to shower the night before surgery and/or the morning of surgery using an antibacterial scrub to prevent infection of the incision sites.
-
If you're pregnant or suspect that you're pregnant, you should tell your surgeon right away.
-
Tell your healthcare provider:
-
If you're sensitive to or are allergic to any medicines, iodine, latex, tape, or anesthesia (local and general)
-
About all prescription and over-the-counter medicines and herbal supplements that you take
-
If you have a history of bleeding disorders or if you're taking any blood-thinning medicines (anticoagulants), aspirin, or other medicines that affect blood clotting. You may need to stop some or all of these medicines before the procedure. Write down which medicines to continue and which medicines to stop, as well as when you should stop them.
-
If you have a pacemaker and other implanted devices
-
Your provider may request a blood test before the procedure to find out how long it takes your blood to clot.
-
If you smoke, you should stop smoking as soon as possible before the procedure. This may improve your chances for a successful recovery from surgery and benefit your overall health.
Based on your health condition, your provider may have other instructions for you.
What happens during an open mitral valve repair?
Heart valve repair surgery requires a stay in a hospital. Procedures may vary depending on your condition and your surgeon’s practices. The operation may take from 3 to 5 hours, and you'll be asleep during the procedure. Generally, heart valve repair or replacement follows this process:
-
You'll be asked to remove any jewelry or other objects that may interfere with the procedure.
-
You'll be asked to remove your clothing and given a gown to wear.
-
You'll be asked to empty your bladder before the procedure.
-
An IV (intravenous) line will be started in your arm or hand. You may be given a dose of IV antibiotics before the procedure starts.
-
Additional catheters may be inserted in your neck and wrist to monitor the status of your heart and blood pressure and to get blood samples. Alternate sites for the additional catheters include under the collarbone and in the groin.
-
You'll be positioned on the operating table, lying on your back.
-
The anesthesiologist will continuously monitor your heart rate, blood pressure, breathing, and blood oxygen level during the surgery. Once you're sedated, a breathing tube will be inserted through your throat into your lungs. You'll be connected to a machine (ventilator) that breathes for you during the surgery.
-
A catheter will be inserted into your bladder to drain urine.
-
The skin over the surgical site will be cleansed with an antiseptic solution.
-
The surgeon will make a cut (incision) down the center of the chest.
-
The sternum (breastbone) will be divided in half with a special operating instrument. The surgeon will separate the 2 halves of the breastbone and spread them apart to expose the heart.
-
To do the valve repair, the heart must be stopped to allow the surgeon to do the procedure. Tubes will be inserted into the heart so that the blood can be pumped through your body by a cardiopulmonary (heart-lung) bypass machine.
-
Once the blood has been completely diverted into the bypass machine for pumping, the heart will be stopped by injecting it with a cold solution.
-
When the heart has stopped, the procedure will begin. The procedure that is done will depend on the type of valve problem that exists. For instance, the procedure may be the separation of fused valve leaflets, repair of torn leaflets, or the reshaping of valve parts to ensure better function.
-
Once the procedure is done, the blood circulating through the bypass machine will be allowed to reenter your heart, and the tubes to the machine will be removed. Your heart will be shocked with small paddles to restart its electrical activity.
-
Once your heart is beating again, the surgeon will watch the heart to assess the function of the heart and the valves.
-
Temporary wires for pacing may be inserted into your heart. These wires can be attached to a pacemaker and your heart can be paced, if needed, during the initial recovery period.
-
The sternum will be rejoined and sewn together.
-
The skin over the sternum will be sewn back together. The incision will be closed with sutures or surgical staples.
-
Tubes will be inserted into your chest to drain blood and other fluids from around the heart. These tubes will be connected to a suction device to drain fluids away from the heart.
-
A tube may be inserted through your nose into your stomach to drain stomach fluids.
-
A sterile bandage or dressing will be applied.
What happens after an open mitral valve repair?
In the hospital
-
After the surgery, you may be taken to the postanethesia care unit (PACU) before being taken to the intensive care unit (ICU) to be closely monitored for a few days. Or you may go right to the ICU.
-
You'll be connected to monitors that constantly display your electrocardiogram (ECG) tracing, blood pressure, other pressure readings, breathing rate, and oxygen level. Heart valve repair surgery generally requires a hospital stay for several days or longer.
-
You'll most likely have a tube in your throat. This is so that your breathing can be helped with a ventilator until you're stable enough to breathe on your own. As you wake up from the anesthesia and start to breathe on your own, the breathing machine will be adjusted to allow you to take over more of the breathing. When you're awake enough to breathe completely by yourself and to be able to cough, the breathing tube will be removed. The stomach tube will also likely be removed at this time.
-
After the breathing tube is out, your nurse will assist you with breathing exercises. These may include coughing (against a firm pillow) and taking deep breaths every few hours. This will be uncomfortable due to soreness, but it's very important that you do this to keep fluids from collecting in your lungs, which could cause pneumonia or other complications.
-
You'll be given pain medicine if you're hurting. You should ask for the medicine before you become extremely uncomfortable. Your nurse will show you how to hug a pillow tightly against your chest while coughing to help ease the discomfort.
-
You may get special IV medicines to help your blood pressure and heart rate and to control any problems with bleeding. As your condition stabilizes, these medicines will be gradually decreased and then turned off when your condition allows.
-
Once the breathing and stomach tubes have been removed and your condition has stabilized, you may start to drink liquids. Your diet may gradually advance to more solid foods as you can tolerate them.
-
When your healthcare provider feels that you're ready, you'll will be moved from the ICU to a post-surgical unit or acute care unit. Your recovery will continue to progress. Your activity will be gradually increased as you get out of bed and walk around for longer periods.
-
Arrangements will be made for a follow-up visit with your healthcare provider.
At home
Once your healthcare providers feel that you have recovered, you'll be discharged home. Follow all instructions from your provider for medicines, pain control, diet, activity, and wound care. Make sure to keep all your follow-up appointments.
Common instructions after surgery may include:
-
Walk as much as possible within reason.
-
Don't do any heavy lifting, pushing, or pulling. Your provider will give you a timeline for certain lifting limits.
-
Gradually go back to normal activities as instructed. Ask your provider about safely returning to work and having sex.
-
You won’t be able to drive a car for a period of time after surgery. This is to allow the sternum and muscles of the chest wall to heal. Ask your provider about when you can start driving again.
-
Watch your wounds for any sign of swelling, redness, bleeding, or discharge. Report these to your healthcare team or get medical care right away.
-
Let your healthcare provider know or get medical care right away about any increasing pain or fever. Call 911 for chest pain or shortness of breath.
-
Eat a heart-healthy diet and maintain a healthy weight. Don't have foods high in fat, cholesterol, and salt. Try to eat a diet rich in fruits, vegetables, and lean meats.
-
Don't smoke. Stay away from secondhand smoke and all tobacco products, including electronic cigarettes.
Keep in mind that your recovery can be slow. It may be anywhere from 4 to 6 weeks or longer before you start feeling better.
Everyone’s situation is different, but the outlook after mitral valve repair is often very good. The outlook may be less positive if your surgeon used more complex methods to fix your mitral valve, or if rheumatic fever had damaged your valve.
If you need dental work in the future, your provider may give you antibiotics to prevent infection of your mitral valve. Before you have any dental procedure, always tell your dentist you've had valve surgery.
Your provider may suggest that you begin a cardiac rehabilitation program. This program gradually reintroduces you to a normal lifestyle. Cardiac rehabilitation begins in the hospital with simple walking and progresses to a regular exercise routine and a nutritious diet. Committing to healthier habits can prevent future heart problems.
Next steps
Before you agree to the test or the procedure, make sure you know:
-
The name of the test or procedure
-
The reason you're having the test or procedure
-
What results to expect and what they mean
-
The risks and benefits of the test or procedure
-
What the possible side effects or complications are
-
When and where you're to have the test or procedure
-
Who will do the test or procedure and what that person’s qualifications are
-
What would happen if you didn't have the test or procedure
-
Any alternative tests or procedures to think about
-
When and how you'll get the results
-
Who to call after the test or procedure if you have questions or problems
-
How much you'll have to pay for the test or procedure