Pacemakers
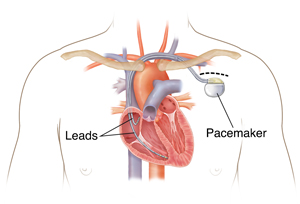
A pacemaker is a small electronic device that keeps your heart rate from going too slow. It makes sure that your heart beats at the appropriate time. Inserting the pacemaker into your body is called implantation. There are several different types of pacemakers. Your healthcare provider will explain which type of pacemaker is best for you.
How do I get ready for a pacemaker procedure?
-
Follow any directions you are given for not eating or drinking before surgery.
-
Tell your healthcare provider about any allergies to medicines, shellfish or iodine contrast, tape or adhesives, or antibiotic soaps. Other options can be provided and precautions can be taken to avoid exposing you to anything that you are allergic to.
-
Follow your healthcare provider's instructions on what medicines to take. If you are taking a blood thinning medicine, your healthcare provider may tell you to stop it before the procedure. This is to decrease the risk of major bleeding. You may be told to stop medicines that interact with the contrast dye that is used during the procedure.
-
You may be asked to shower with antibacterial soap the night before your procedure and the morning of the procedure. Ask your healthcare provider what kind of soap to use.
-
Your healthcare provider may ask you to use clean bed sheets and pajamas the night before the procedure. This can reduce the risk of infection.
-
You may be given an antibiotic through an IV (intravenous) line to also protect you from infection after the implant procedure.
-
You will have blood drawn depending on your overall health. If your kidneys are not healthy, special care may be needed before the procedure.
-
If you are a woman of child-bearing age, you may be asked to take a pregnancy test before the procedure.
What happens during the procedure?
-
Your healthcare provider may prescribe a medicine to help you relax and to prevent pain during the procedure.
-
An IV line will be placed in the arm on the same side of the procedure site.
-
A local anesthetic is given by injection to numb the area where the pacemaker will be inserted. This keeps you from feeling pain during the procedure.
-
The healthcare provider will make a cut (incision) where the generator is placed.
-
The healthcare provider will guide the wire (lead) through a vein into your heart’s chambers using X-ray monitors.
-
The healthcare provider will attach the pacemaker generator to the lead or leads and test the device.
-
The healthcare provider will close the incision site with stitches. They may also seal the site with a surgical glue to prevent infection.
-
A dressing may be applied to your incision. This is to reduce the risk of bleeding and protect it from infection.
-
The pacemaker’s settings are programmed to help your heart beat at a rate that’s right for you.
What happens after the procedure?
-
You will have a chest X-ray while you are in the recovery area.
-
Your pacemaker settings will be rechecked.
-
Your healthcare provider may prescribe antibiotics to take after the procedure to prevent infection.
-
Follow the instructions you are given for caring for the implantation site. You may be told not to raise the arm on that side for a certain period. You may have a sling to keep you from moving your arm on the incision side. This is done to prevent the new pacemaker wire from becoming displaced. Your healthcare provider will tell you how long and when you should wear this.
-
Take your temperature and check your incision for signs of infection every day for a week.
-
Return for a follow-up visit as advised.
-
Ask your healthcare provider when it will be safe to shower, bathe, or swim. Generally, you should not soak in water for about a week to prevent the incision from softening, opening, or becoming infected.
-
Don't do any activities that would put pressure on your incision site or cause irritation to the incision. Don't use lotions, powders, or ointments unless your healthcare provider says it's OK. Don't carry a purse or backpack that would put pressure on your incision site.
Pacemakers and electronics
Be careful when using cell phones and other electronic devices. Keep them at least 6 inches away from your pacemaker. It's safest to hold all cell phones to the ear farther from your pacemaker or use the speaker mode setting. Don’t carry your phone or electronic device in your chest pocket, over the pacemaker. Experts advise carrying your cell phone and other electronics in a pocket or bag below your waist. Most cell phones and electronic devices don't interfere with pacemakers. But some cell phones and electronic devices such as smart watches use powerful magnets for wireless charging. These may interfere with the normal function of your pacemaker. The magnet used for charging or other magnet accessories can also interfere with the normal function of your pacemaker. These devices should be kept at least 12 inches away from your pacemaker when wirelessly charging or stored. Follow any other instructions given to you by your healthcare provider or from the manufacturer of your pacemaker.
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following:
-
You feel any of the symptoms you had before the pacemaker was implanted, such as lack of energy.
-
Your chest or abdominal muscles twitch.
-
You have hiccups that won't stop.
-
You have a rapid or pounding heartbeat or shortness of breath.
-
You feel pain in the area around your pacemaker.
-
You have a fever of 100.4°F (38°C) or higher (or 1 degree or higher above your normal temperature) , or as directed by your healthcare provider.
-
You have redness, severe swelling, drainage, bleeding, or warmth at the incision site.
-
Your incision site is not healing, or it separates or opens.
-
Your pacemaker generator feels loose or like it is wiggling in the pocket under the skin.
-
You need an MRI for any reason. In some cases, it's not safe to have an MRI with a pacemaker.
Call 911
Call 911 if you have:
Online Medical Reviewer:
Ronald Karlin MD
Online Medical Reviewer:
Stacey Wojcik MBA BSN RN
Online Medical Reviewer:
Steven Kang MD
Date Last Reviewed:
7/1/2023
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.