Mastectomy with Reconstruction
Mastectomy is surgery to remove a breast. It’s most often done to treat breast cancer. Double (bilateral) mastectomy is when both breasts are removed. It might also be done to decrease the chance of breast cancer in certain women at high risk.
After a mastectomy, you may choose to have reconstruction surgery to rebuild the breast shape. Reconstruction can be done using breast implants or tissue from another part of the body. Sometimes a combination of both is used. The tissue can come from the belly, buttocks, inner thigh, or back.
Mastectomy and reconstruction can be done at the same time. (This is called immediate reconstruction.) Or they may be done as two separate surgeries. Reconstruction is planned for later (delayed reconstruction) so your body can heal in between. You may need more surgeries at a later time to complete the reconstruction.
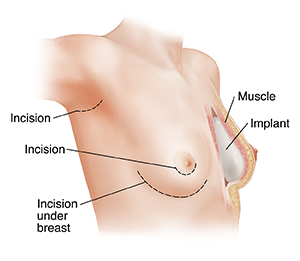 |
| Breast implant (showing possible incisions). |
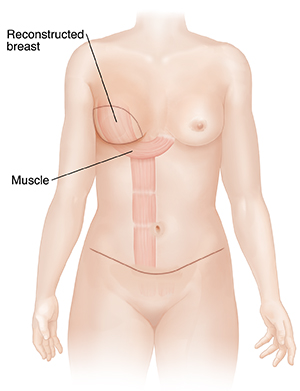 |
| Flap reconstruction. |
Getting ready for surgery
You'll get instructions on how to get ready for surgery. Be sure to:
-
Tell your healthcare provider about all medicines you take. This includes prescription medicines, over-the-counter medicines, herbs, vitamins, and other supplements. It also includes marijuana, CBD, and street drugs. You may need to stop taking some or all of them before surgery.
-
Quit smoking. Smoking makes it harder for you to heal. Ask your healthcare provider for help quitting.
-
Get your pre-op tests. A few days before surgery, tests will be needed to get an idea of your overall health and be sure you are well enough for surgery. These might include blood and urine tests and an ECG (electrocardiogram) to check your heart.
-
Follow any directions about not eating or drinking before your surgery. This includes coffee, water, gum, and mints. If you have been told to take your usual medicines, take them with a small sip of water.
The day of surgery
The length of surgery depends on the type of mastectomy surgery and type of reconstruction to be done. Ask how long your surgery is expected to take. You'll stay in the hospital after the surgery. How long you're there depends on the type of surgery you had, your overall health, and how well you recover. Your treatment team will talk with you about the details of your surgery, but below is a brief overview of what you might expect.
Before surgery starts
-
An IV (intravenous) line is put into a vein in your arm or hand. This is used to give you fluids and medicines.
-
A blood pressure cuff will be put on your arm, and you'll be hooked up to a heart monitor. These are used to make sure you're OK during surgery.
-
Medicine is given so you sleep and don't feel pain during surgery. This is called general anesthesia. A tube may be put into your throat to help you breathe.
During mastectomy
-
Medical staff will clean your skin. They will put sterile drapes around you to help prevent infection.
-
The surgeon will make one or more cuts (incisions). In most cases, the surgeon will remove all of the breast tissue, the skin over the breast, and the nipple. In some cases, most of the skin and nipple may be preserved.
-
The surgeon may also remove lymph nodes near the tumor. These will be checked for cancer. Lymph nodes are small masses of tissue that are part of the body’s immune system. If your lymph nodes contain cancer, you'll likely need other treatments after surgery.
During reconstruction
-
For breast implants, a silicone sac filled with silicone gel or saline (saltwater) is used to form the shape of the breast. The surgeon usually places the implant under the chest muscle. If there's not enough space to put in the implant, they may put in a tissue expander. This is an empty implant that is slowly filled over time to gently stretch the skin and muscle so there's space for a permanent implant. The tissue expander is then removed and an implant is put in at a later time.
-
For flap reconstruction, the surgeon takes tissue from another part of your body to rebuild the breast shape. The tissue might come from your belly, back, buttocks, or thighs. Sometimes an implant is also used. Flap reconstruction means you'll have two surgical sites: your chest and the part of your body where the flap was taken.
-
The surgeon may build a nipple and the dark area around the nipple (areola) during or after the surgery.
-
Soft plastic tubes (called drains) will be put into the incisions. These help to drain out extra fluid that can build up as you heal. The incisions are then closed with staples or sutures (stitches). Bandages will then be wrapped around your chest.
After the surgery
You will be taken to a room to wake up from the anesthesia. You may feel sleepy and nauseated. If a breathing tube was used, your throat may be sore for a little while. You’ll be given medicine to manage pain. Tell your healthcare providers if you have pain.
When you’re ready, you’ll be moved to a room to stay for one or more nights. Before you leave the hospital, your healthcare team will show you how to care for your bandages and drains.
When it’s time to go home, you'll need an adult family member or friend to drive you home. Prepare to have someone stay with you for the first few days, to help at home while you heal.
Recovering at home
Once you are home, follow any instructions you are given. Your healthcare provider will tell you when you can return to your normal routine. During your recovery:
-
Take your pain medicine as directed. Ask about side effects it could cause and what you can do to manage them. Good pain control allows you to move and take deep breaths to speed your recovery.
-
Eat normal meals as soon as you feel able. Stick to a healthy, well-balanced diet.
-
Prevent constipation. Eat fruits, vegetables, and whole grains. Drink 6 to 8 glasses of water a day, unless directed otherwise. Use a laxative or a mild stool softener if your healthcare provider says it’s OK.
-
Rest when you are tired. Don’t worry if you are extremely tired (fatigued). Fatigue and weakness are normal for a few weeks. This will get better over time.
-
Care for your incisions and bandages as instructed by your healthcare provider. Remember, if you have flap surgery, you will have two surgical wounds: the chest and the part of the body the flap was taken from.
-
Follow your healthcare provider’s guidelines for showering. Don't swim, take a bath, use a hot tub, or do anything that would cover your incisions with water. Wait until your healthcare provider says it’s OK.
-
When you're allowed to shower, gently wash your incision sites. Then pat the incisions dry. Don’t put lotions, oils, or creams on them until they are fully healed.
-
Don’t drive until you're no longer taking prescription pain medicine and your healthcare provider says it’s OK. This is usually at least 10 days. When riding in a car, carefully position the seatbelt so it doesn’t go across your breasts.
-
Care for your drains as directed. You may need to empty them at least every 8 hours. You may be asked to measure the fluid that comes out. The amount of fluid will decrease over time.
-
Your healthcare provider will talk with you about ways to manage swelling around your incisions. Follow instructions as directed.
-
Walk as often as you feel able.
-
Be sure you understand what you can and can't do. Don't lift anything heavy or do housework until your healthcare provider says it's OK. Ask when it's OK to go back to work.
-
Do exercises as directed. Breathing exercises can help prevent pneumonia. Others help prevent swelling, keep your arm and shoulder joints flexible, and improve circulation. For instance, you may be told to squeeze a rubber ball with your hand or lift your arm out to your side. You may also need physical therapy after reconstruction. This is to strengthen the muscles affected by the surgery.
Wearing a breast prosthesis
A breast form (prosthesis) is a soft, breast-shaped form that fits into a bra. You may decide to use a breast prosthesis if reconstruction isn’t done at the same time as the mastectomy. Or you may use one if you choose not to have reconstruction. Some women wear breast forms to help balance weight and not have back strain. Other women wear them because they like the way they look. Talk with your healthcare provider if you want a prescription for a prosthesis.
When to call your healthcare provider
Talk to your healthcare provider about problems you should watch for. Call right away if you have any of the following:
-
Extreme chest pain or trouble breathing ( call 911 or other emergency service)
-
A fever of 100.4°F ( 38°C ) or higher, or as directed by your healthcare provider
-
Chills
-
A change in pain, redness, swelling, or bleeding at the incision site
-
Incision opens up or the edges pull apart
-
A change in the way the drainage looks or increased drainage
-
Swelling in your hand, arm, or chest that gets worse or is not getting better a week or two after surgery
-
Cough or shortness of breath
-
Pain, redness, swelling, or warmth in an arm or leg
-
Pain that’s not managed by medicine or gets worse
-
Increasing pain in or around your incisions
-
Bleeding that soaks through the bandage
-
Trouble passing urine or changes in how your urine looks or smells
-
Any other problems your healthcare provider told you to watch for and report
Know how to reach your healthcare provider any time problems come up. This includes after office hours, on weekends, and on holidays.
Follow-up care
You will have follow-up appointments with your healthcare provider. If you have stitches (sutures) or staples that need to be removed, this may be done 7 to 10 days after surgery. Drains may be removed within 2 weeks. You may need to schedule more surgery for nipple and areola reconstruction. Or you may need surgery to match the remaining breast to the reconstructed one (if only one breast was affected). If you have any questions or concerns about your recovery, let your healthcare provider know.
Your long-term recovery
To help you cope with the loss of your breast, you may want to meet with a psychologist or other healthcare provider for counseling. It may also help to talk with family members and friends. Think about joining a support group as well. You may find it easier to talk with women who are going through experiences like yours.
Risks and possible complications
Any type of surgery has some risk. Some problems related to mastectomy with reconstruction include:
-
Infection
-
Bleeding
-
Fluid collection (seroma) or blood collection (hematoma)
-
Pain or numbness
-
Long-term swelling of the chest, arm, or hand (lymphedema)
-
Scarring
-
Hardening of the breasts or damage to breast tissue
-
Problems with breast implants that mean they have to be replaced
-
Problems with wound healing
-
Loss of the tissue flap. This may lead to more surgery and possible implant removal if present.
-
Muscle weakness, lumps of fat tissue at the flap donation site, or hernias (abdominal flap reconstruction only)
-
Not being happy with how you look after the procedure
-
Risks of anesthesia (the anesthesiologist will discuss these with you)
Talk with your healthcare provider about the risks related to your surgery and what you can do to help prevent problems.